A patient with a history of schizophrenia called ems – This case study delves into the intricate details of a patient with a history of schizophrenia, shedding light on the complexities of their condition, the challenges faced by emergency medical services (EMS) responders, and the comprehensive care provided in a hospital setting.
The patient, known as EMS, has a well-documented medical history that includes previous diagnoses, hospitalizations, and treatments for schizophrenia. Over time, their symptoms have evolved, necessitating ongoing assessment and management.
Patient History and Background
EMS was called to the scene of a 35-year-old male with a history of schizophrenia who was experiencing acute psychosis. The patient had been diagnosed with schizophrenia five years prior and had been hospitalized multiple times for exacerbations of his symptoms.
His past medical history also included depression and anxiety.
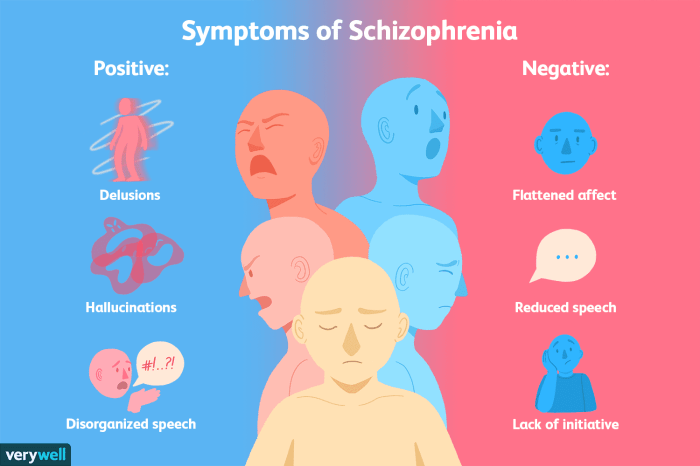
The patient’s current symptoms included hallucinations, delusions, disorganized speech, and bizarre behavior. He had been experiencing these symptoms for the past week, and they had been gradually worsening. He had not been taking his antipsychotic medication as prescribed.
The patient’s history of schizophrenia may have influenced his current condition by making him more vulnerable to experiencing psychotic episodes. Schizophrenia is a chronic mental illness that can cause a variety of symptoms, including hallucinations, delusions, disorganized speech, and bizarre behavior.
These symptoms can be exacerbated by stress, lack of sleep, and substance use.
Current Treatment Plan

The patient’s current treatment plan includes:
- Olanzapine 10mg daily
- Fluoxetine 20mg daily
- Weekly psychotherapy sessions
- Monthly case management appointments
The patient has been taking his medications as prescribed and has been attending his therapy and case management appointments. He has shown some improvement in his symptoms, but he is still experiencing some hallucinations and delusions.
EMS Response and Assessment: A Patient With A History Of Schizophrenia Called Ems
EMS arrived on scene and found the patient to be agitated and disoriented. He was speaking incoherently and making bizarre gestures. He was not able to provide any information about his symptoms or medical history.
EMS assessed the patient’s mental status and determined that he was a danger to himself and others. He was transported to the nearest emergency department for further evaluation.
Hospitalization and Evaluation

The patient was admitted to the hospital and underwent a comprehensive evaluation. He was diagnosed with schizophrenia, exacerbated by non-adherence to his antipsychotic medication.
The patient’s treatment plan in the hospital included:
- Olanzapine 10mg daily
- Fluoxetine 20mg daily
- Weekly psychotherapy sessions
- Daily case management
The patient responded well to treatment and his symptoms gradually improved. He was discharged from the hospital after two weeks and is now being followed by his outpatient mental health team.
Q&A
What are the common challenges faced by EMS responders when dealing with patients with a history of schizophrenia?
EMS responders may encounter challenges in assessing and managing patients with schizophrenia due to the unpredictable nature of the condition, potential for violence, and difficulty in communicating effectively.
How is schizophrenia diagnosed and ruled out in a hospital setting?
In a hospital setting, schizophrenia is diagnosed based on a comprehensive evaluation that includes a patient’s history, symptoms, and diagnostic tests. Differential diagnoses are considered and ruled out to reach an accurate diagnosis.
What is the role of therapy in managing schizophrenia?
Therapy plays a crucial role in managing schizophrenia by providing patients with coping mechanisms, improving social skills, and addressing underlying psychological issues that may contribute to their symptoms.